|
|
|
|
|
||
|
||
|
1 9 - 1 1 - 2 0 0 5 Sudden cardiac death during anabolic steroid abuse: morphologic and toxicologic findings in two fatal cases of bodybuilders
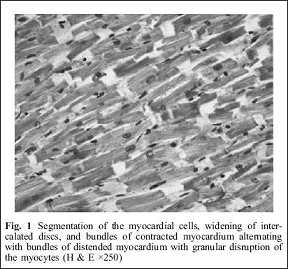
Fineschi V, Riezzo I, Centini F, Silingardi E, Licata M, Beduschi G, Karch SB. A consensus is beginning to emerge that chronic AAS abuse may be associated with an increased risk of sudden cardiac death (SCD), myocardial infarction, altered serum lipoproteins, and cardiac hypertrophy. To further examine the relationship between AAS and SCD, we report two cases of sudden cardiac death that occurred in previously healthy bodybuilders taking AAS at the time of death. In both cases, we were able to perform an autopsy, histology of the organs, and toxicologic analysis. Case 1 A 29-year-old bodybuilder suddenly collapsed after dinner in his apartment. He had a weight lifting workout at the gymnasium a few hours before. Cardiopulmonary resuscitation initiated by an emergency physician was unsuccessful. According to friends of the deceased, he had been taking anabolic steroids (testosterone, nandrolone, and stanozolol) parenterally for several years mainly in an effort to improve his appearance. Several glass vials were found in his room and were labeled Winstrol (stanozolol), Deca (nandrolone), Testoviron Depot, and Andriol (testosterone). At autopsy, the body weighed 72 kg, and the length was 166 cm [body mass index (BMI), 26.1]. The decedent had a muscular build, and there were no external signs of injury. Apart from the heart, all other organs were macroscopically normal. The heart had a normal shape and weighed 380 g, with a predicted weight of 304 g (range 215–429 g). The coronary arteries were normal. The myocardium and the valvular apparatus were normal. Both ventricular wall thicknesses were normal. Samples of the atria and ventricles (n=10) were taken, fixed in 10% buffered formalin, and embedded in paraffin. Microscopic examination revealed numerous foci of contraction band necrosis. There were two microfoci of fibrosis, one in the subendocardial anterior left ventricle and one in the interventricular septum. Segmentation of the myocardial cells and/or widening of intercalated discs and bundles of contracted myocardium alternating with bundles of distended myocardium with granular disruption of the myocytes were noted in all myocardial sections.
Examination of the conduction system performed according to Sheppard and Davies was unremarkable. The coronary arteries were normal along their entire course, showing only the physiologic intimal thickening typical of the subepicardial arterial vessels. The remainder of the histological examination was unremarkable. Complete toxicologic examination was negative for drugs of abuse, including ethanol, but multiple AASs were detected by comparison of each spectrum with the instrument's National Institute of Standards and Technology (NIST) Library. The positive results for nandrolone, stanozolol, and their metabolites were confirmed with AAS standards supplied by SALARS and Sigma. The urine concentration was for nandrolone not measurable, stanozolol 43 µg/l, and testosterone/epitestosterone ratio (T/E)=28.7.
Case 2 A 30-year-old male, first an amateur, and later a competitive bodybuilder, who worked out regularly at the gymnasium, suddenly collapsed at home and was pronounced dead by an emergency physician who does not start cardiopulmonary resuscitation. He had a weight lifting workout at the gymnasium a few hours before. In an ashtray near the body, a 2-ml vial of nandrolone decanoate was found along with a used 2.5-ml syringe. The apartment contained a veritable arsenal of drugs, most of which fell into the AAS category. All witnesses confirmed that the subject had started using AAS approximately 6 months prior to his death. Baseline blood tests, performed a few days before death, were unremarkable except for a slight increase in hepatic enzymes. The body was that of a well-built man (weight 90 kg, length 178 cm, and BMI=28.4). External examination revealed a needle mark on the upper external part of the right buttocks. The autopsy revealed abnormal muscle development, testicular atrophy, and hepatomegaly. The heart weight was 400 g. The wall thicknesses were normal. Coronary arteries showed scattered fatty streaks. Histopathologic examination of the heart revealed focal myocardial fibrosis; examination of the conduction system performed according to Sheppard and Davies was unremarkable. The liver showed cholestasis and vascular gaps compatible with the diagnosis of peliosis hepatis.
Tests for narcotics, psychotropic drugs, and for ethanol were negative. Screening for anabolic agents was done using the examination procedure proposed by Karch. Urine screening revealed the presence of norandrosterone, and blood test was also positive for nandrolone. TE ratio was 42. The total absence of hair in the whole body did not allow the relevant tests to be carried out.
Discussion In both cases, the morphologic findings are, in combination with the toxicologic findings, sufficient to explain the deaths as related to the cardiac effects of AAS abuse. In both cases, blood and/or urine revealed the presence of nandrolone and its principal metabolite (19-norandrosterone). A thorough scene investigation documents the subjects' use of stanozolol and nandrolone (presumably 'nandrolone decanoate' as found in the ashtray). Because the metabolite was not normalized to the creatinine ratio, little can be concluded about the urine concentration, but the values found here are comparable to previously reported values. The high testosterone/epitestosterone ratio supports our hypothesis that testosterone was the form of the abused drug. Hepatic diseases in athletes and bodybuilders after abusing AAS have been reported. Hepatic injury, including cholestasis, peliosis hepatis, hyperplasia, and tumors, have been attributed to abuse of the 17a-alkylated AAS. In the present case, cholestasis injury induced by AAS consisted mainly of bile accumulation in the cytoplasm of the liver cells and of bile casts in canaliculi, but without evidence of inflammation or necrosis. Peliosis hepatis is defined as cystic blood-filled spaces in the liver. Microscopic peliosis hepatis is often confused with extreme sinusoidal dilatation or with evacuation of the liver cell plates, a lesion seen after zonal hepatocellular dropout but without loss of the normal reticulin fibers. To be called peliosis hepatis, lesions should have evidence of rupture of these fibers. In our case, lesions were randomly distributed without zonal preference. The available literature examining the cardiovascular effects of AAS share some common features. Abuse of AAS can induce alterations in lipoprotein metabolism that may predispose to myocardial infarction. The presence of androgen receptors in human cardiac myocytes in both sexes and the fact that androgens can directly mediate a significant hypertrophic response in cardiac myocytes have been demonstrated. Vascular endothelial cells may be directly affected by AAS, which may result in vasospasm. Moreover, the fact that abusers take a bewilderingly large number of steroid products, in various forms, singly and in different temporal combinations and sequences, makes interpretation of pathologic findings extremely difficult. In the present cases and in all but one of the published reports, the coronary arteries were free of atheroma, and there was no evidence of thrombi. We did not find myocardial hypertrophy; therefore, we were unable to confirm the suggestion that AAS toxicity is manifested mainly as myocardial hypertrophy. It has recently been proposed that body builders taking AAS experience sustained increases in heart rate and blood pressure that may result in compensatory hypertrophy of the left ventricular wall, but it is unclear how one would distinguish hypertrophy due to AAS and hypertrophy due to exercise itself. The proportion of these increased physiological parameters attributable to AAS, as opposed to that resulting from the exercise itself, is unclear, and three recent studies of bodybuilders taking AAS did not demonstrate significant cardiac hypertrophy. It is, however, agreed that when AAS abuse is coupled with intense exercise training, concentric hypertrophy of the left ventricular wall and impaired diastolic function may result. Drug-free vigorous weight training will also increase left ventricular wall thickness and mass but will not hinder cardiac function. However, when combined with anabolic steroids, cardiac hypertrophy could become pathologic. There are additional steroid-related pathophysiologic mechanisms that might have played a role in causing the cardiac pathology noted here. Four hypothetical models of how AAS abuse might induce adverse cardiovascular effects (atherogenesis, thrombosis, coronary artery vasospasm, and direct injury models) have been proposed. Our findings were consistent with the direct injury model. Indeed, the heart expresses androgen receptors and would, therefore, be directly influenced to some degree by AAS. We have previously reported focal myocardial necrosis in AAS users, namely, coagulative myocytolysis (or contraction band necrosis), typical of catecholamine myocytotoxicity, linked with ventricular fibrillation and sudden death. The described focal fibrous area could be interpreted as the healing phase, with progressive collagenization ending in a fibrous scar of previously focal myocell necrosis. From these findings, it can be concluded that anabolic steroids and exercise lead to a stimulation of the sympathetic nervous system. Recently, it has been described that the combined effect of exercise and anabolic steroids causes an overstimulation followed by a transient functional and structural destabilization of the sympathetic axon terminals; the transient destabilization of sympathetic axon terminals could be suggested as a reason for increased vulnerability to ventricular fibrillation. Our cases support the hypothesis that the combined effects of vigorous weight training, anabolic steroid use, and androgen sensitivity may have predisposed these young men to myocardial injury and subsequent sudden cardiac death. We would reinforce the warning against use of these drugs by athletes and heightened surveillance for AAS-related death that may be underrecognized and underreported in the medical literature. |
|
|